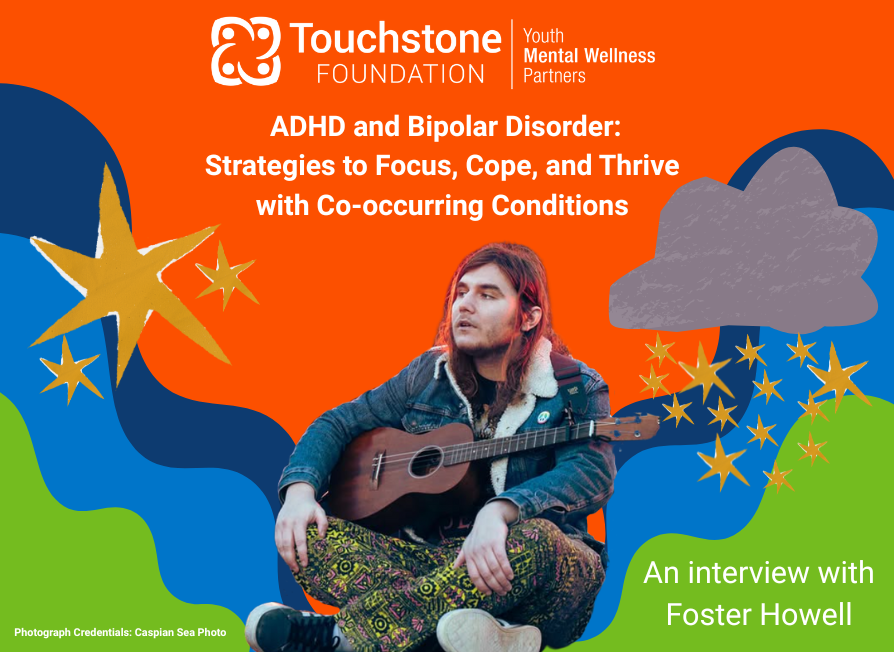
ADHD and Bipolar Disorder: Strategies to Focus, Cope, and Thrive with Co-occurring Conditions
“My mom would tell me to write everything down. It didn’t work because I’d have to remember to write it down.”
– Foster Howell
It’s a funny line—until you realize how perfectly it captures the everyday reality of ADHD.
For Foster Howell, a member of our community, that line wasn’t just a quip. It was a snapshot of daily life. For much of their life, strategies meant to “fix” things never quite stuck—not because they weren’t trying, but because something deeper was at play.
For many, including Foster, a late diagnosis feels like finally getting the answer to a question they didn’t even know how to ask. Their story highlights how easily ADHD can be overlooked—especially when it doesn’t match the stereotype.
What ADHD Doesn’t Look Like
“ADHD is a little misleading because it’s not necessarily a deficit of attention,” Foster shared. “We can pay attention well to some things. We just don’t have the ability to regulate when we will have the capacity to pay attention. Our brain doesn’t regulate attention well.”
When people picture ADHD, they often imagine a hyperactive child bouncing off the walls, blurting out answers, or interrupting constantly. But ADHD doesn’t always look like that—and that narrow image often does more harm than good.
“I was very inattentive type,” Foster said. “I wasn’t physically hyperactive, and that’s kind of what my parents understood ADHD to be.” Their teachers thought they weren’t trying. Their parents didn’t know what to do—not because they didn’t care, but because they didn’t recognize the signs.
That mismatch between perception and reality can be isolating. Foster shared how difficult it was to advocate for themselves when the world expected a different version of ADHD.
Expert Insight: Why Diagnosis Is Complicated—and Personal
To better understand Foster’s journey, we spoke with Dr. James G. Waxmonsky, a Professor of Psychiatry and Behavioral Health and Chair of Child Psychiatry at Penn State University.
“There’s no blood pressure cuff for the brain,” he said. “The field is working on it, but right now, there’s no mental health strep test to guide us.”
That lack of objective testing makes it hard to differentiate between similar disorders—like ADHD and Bipolar Disorder.
“Both present with issues staying on task,” he explained. “With Bipolar Disorder, we look for mood changes in addition to focus problems, but people with ADHD can become depressed from the repeated frustration of falling behind.”
Dr. Waxmonsky stressed that diagnoses aren’t always “clean,” and treatment can’t always be guided by labels alone. Instead, it has to start with the person seeking care.
“The most useful information in mental health is what the patient has to say. The best test is face-to-face time. Effective treatment is a collaboration. The goal needs to come from the patient.”
In Foster’s case, that goal was clarity, functioning, and peace of mind—even if medication wasn’t a fit.
Dr. Waxmonsky encourages people to set daily, tangible goals—not vague aspirations like “feel less anxious.”
“Can you get the kids to bed by 9 p.m. four nights a week? Can you get 30 minutes of writing done after work? Can you spend less than 30 minutes a day stuck in a worry cycle?”
These are the metrics that make progress real. Specific goals not only help track what’s working—they reveal what might need to change.
“It’s really hard to improve organizational skills with a medicine,” he noted, “but several counseling programs are designed to help with that for people with ADHD or Bipolar Disorder.”
When One Diagnosis Becomes Two: Co-Occurring Conditions
A diagnosis of ADHD can bring clarity. But when it comes with a second diagnosis—like bipolar disorder—that clarity often becomes complicated.
For many people, ADHD doesn’t exist in a vacuum. Co-occurring conditions such as anxiety, depression, or learning differences can make treatment more complex. And when symptoms overlap, the path forward isn’t always clear.
For Foster, their bipolar 1 diagnosis came during a mental health crisis. Everything changed.
“If you have both bipolar and ADHD,” they explained, “the bipolar is the one that gets priority. You have to treat that first. ADHD becomes secondary.”
That prioritization can feel defeating—especially when both conditions deeply impact daily functioning. Foster tried revisiting ADHD treatment with a non-stimulant medication (Strattera), but the side effects caused a return of instability.
“I was sobbing at the psychiatrist’s office,” they said. “I didn’t think there was any hope for me to be successful.”
This emotional crossroads is familiar for many with co-occurring conditions: being told to manage one part of the brain while sidelining another. Foster’s story shows why awareness and nuanced care are vital—not just to diagnose, but to understand.
Navigating ADHD Without Medication
When ADHD medication isn’t effective—or needs to be paused to manage other conditions—it’s easy to feel stuck. But “no meds” doesn’t have to mean “no hope.”
“I did research for myself,” Foster said. “I’m a lot better at addressing my ADHD symptoms without medication.”
One key resource for them? How to ADHD by Jessica McCabe.
“It breaks down the science and symptoms of ADHD in an understandable way,” Foster said. “And it gives you strategies you can use—even without medication.”
To help stay focused, Foster chose the audiobook version. For many with ADHD, listening can make absorbing information easier than reading.
Therapy also became essential. While it isn’t a universal fix, it offered Foster tools for emotional regulation and navigating the unique challenges of overlapping conditions.
“You can just do things in your own weird, different way,” they said. “And there’s nothing wrong with that. It’s just different.”
“You can survive in this very difficult-to-navigate world and be just fine—even if you have to do things a little bit differently.”
That part? Worth repeating.
Building a Personal Toolkit: Foster’s Go-To Strategies
Foster’s journey wasn’t linear—and it wasn’t always easy. But through self-education, therapy, and flexibility, they built a toolkit that works for them.
Here are a few of their go-to strategies:
- Accessible education: Foster recommends How to ADHD by Jessica McCabe, especially the audiobook format for those who find traditional reading challenging.
- Self-advocacy through research: Learning how their brain works helped Foster reframe their challenges and identify strategies that actually stick.
- Therapy: It provided essential support for navigating emotions and learning practical coping skills.
- Reframing success: Foster emphasizes that your version of success doesn’t have to look like anyone else’s. What works for you is enough.
Sometimes, ADHD is quiet. Sometimes, it hides behind missed deadlines or misunderstood emotions. But with awareness, support, and the right tools, people with ADHD—and co-occurring conditions like bipolar disorder—can flourish.
Foster’s story is a powerful reminder: no one should have to navigate neurodivergence alone.
Whether you’re a teacher, a parent, a friend, or someone just beginning your journey—keep listening. Keep learning. And don’t be afraid to do things a little differently.
After all, who gets to say what “normal” looks like, anyway?